One of the biggest obstacles facing a laboring mother who is attempting to minimize interventions is the external fetal monitor. Most hospitals require it continuously rather than checking every half hour or so. That means that you will be strapped to the bed.
This is truly a enormous problem. Being strapped down seriously limits your movement, and movement passes time, keeps endorphins flowing, and helps your baby wiggle around to find the best position. And then of course there are the psychological benefits of movement; most notably feeling like you are able to work with the contractions and not merely be subject to them.
So what do you do? Obviously it is very important to monitor the baby's heart rate, but is it necessary to do it continuously? In "Childbirth Instructor Magazine", Leah Albers CNM, DrPH said:
"Many parents and health professionals believe that serious labor complications cause fetal asphyxia and that fetal asphyxia can cause permanent brain damage such as cerebral palsy in the newborn. Those who believe that by identifying perinatal asphyxia, EFM (external fetal monitoring) can prevent neurologic impairment have unrealistic expectations of this technology. In fact, EFM has not decreased the incidence of cerebral palsy. Over the past 40 years, the rate of cerebral palsy has not changed and remains at about 2 per 1,000 live births."
So then, should we just get rid of fetal monitoring? Not at all. Fetal monitoring is extremely important in helping to prevent all sorts of things. Even midwives at home births monitor the heart rate from time to time throughout labor. Keeping a constant eye on your baby does not seem completely necessary, however.
Regardless of what your wishes are with all that, your hospital will have specific policies about fetal monitoring. Keeping it on continuously has great advantages for them; they will have the entire labor mapped out with a written record of every contraction and every beat of your baby's heart, which is very useful if ever the hospital is taken to court. Continuous montoring is also less work for the nurses, so if they happen to have many laboring women at once they can keep a better eye on them.
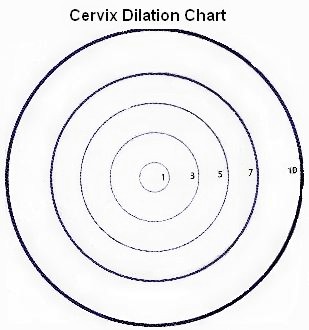
More than likely your hospital will require you to have the monitor on. I know I have talked it down so much that you are probably terrified ... but don't despair! There is still much you can do with the monitor on. Be sure that at least you switch sides you are lying on in bed, but if you are able, you can also set up a chair next to the bed and move to that, which will get gravity on your side. You can also have your husband or birth partner stand next to the bed while you lean on him. You can lay the bed flat and get on all fours, which will take a lot of pressure off your back. And you can ask to be unhooked and go to the bathroom every couple of hours. You should be doing this not only for the chance to walk; it will also keep your bladder flat so the baby can put as much pressure as possible on your cervix to open it more quickly. And if you can stand it (it often seems to cause contractions to become more frequent), stay and labor on the toilet. It is really helpful, because you will have more contractions while at the same time keeping your pelvic floor loose, so things should open up more quickly.
Learn what the procedures are at your place of birth, and talk to your nurses. They need to follow the hospital guidelines, but they are usually more than willing to work with you and can come up with some great, unique positions to labor in.